From Plant Hybrids to Human Health: A Novel Path to Biomedical Innovation
Krishna Ella’s unconventional pathway to the biomedical field has led to greater access to vaccines in the developing world.
Interview by Nik Hawkins for Grow Magazine, College of Agricultural & Life Sciences, University of Wisconsin–Madison.
April 8, 2022
Krishna Ella is pictured among potato plants in the Walnut Street Greenhouse during a visit to the UW campus in May 2022. Ella remembers fondly the months he spent at the Hancock Agricultural Research Station harvesting and weighing potato tubers for protoplast fusion research. “You don't get that in the classroom,” Ella says. “Unless you touch the soil, unless you harvest a potato, you don't have a feel for what a farmer is doing. And that touch is very critical.” Photo by MICHAEL P. KING
When Krishna Ella PhD’93 arrived at CALS in 1987 to begin a doctoral program in plant pathology, his goal was to probe the mysteries of hybrid plants. He wanted to use that knowledge to help farmers in their fields. But an understudied cellular process captured his attention and ultimately redirected him to the medical sciences.
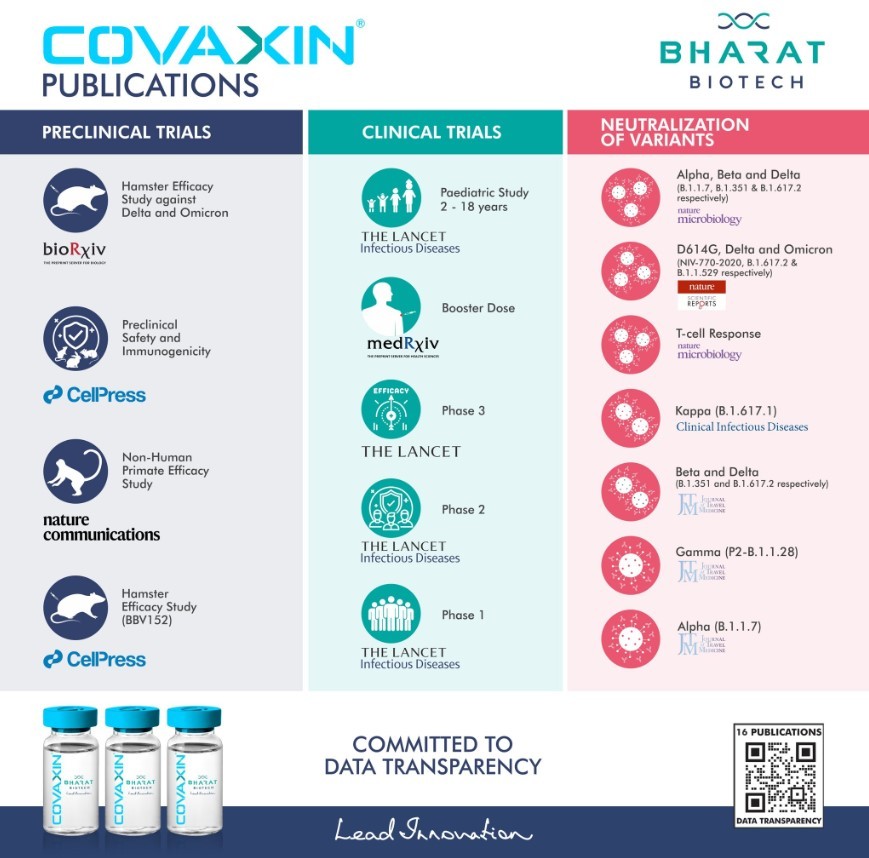
About a decade later, Ella and his wife, Suchitra, returned to India and founded Bharat Biotech in Hyderabad. Since that time, it has grown into a multinational biotechnology company that develops new vaccines and biotherapeutics. Bharat Biotech now holds 145 global patents, boasts a portfolio of 16 vaccines, and has delivered more than 5 billion vaccines worldwide, with a primary focus on the developing world. The company is a leader in pandemic vaccines, and its products have been prequalified for use by the World Health Organisation.
UW has recognised Ella’s accomplishments with the Distinguished Alumni Award in 2011 and an honorary degree in 2022, which he accepted at commencement in May. In this special alumni edition of Living Science, we catch up with Ella to talk about his academic path, what he gained from his time at CALS, and his goals for Bharat Biotech.

What led you to study plant pathology at CALS?
I chose UW because the plant pathology department [at CALS] was one of the best in the world. And I liked the diversity that was happening in the department — the type of faculty, their ideas, the purely applied aspect of it. Truly useful to farmers
How did your academic plans change after you arrived at CALS?
I came for my Ph.D. to study protoplast fusion with [now professor emeritus] John Helgeson; but, somehow, after one year, I lost interest in that. At the time, signal transduction was well understood in bacteria, how bacteria can sense the environment and their surroundings, but nothing was understood about how plants and pathogens can interact. So, I told John I wanted to work on signal transduction — protein kinases, phosphorylation, dephosphorylation, and what makes differences in the disease. That was research that absolutely nobody was working on in the entire world.
Protoplast fusion is a form of genetic modification used to combine two distinct plant species into a hybrid plant that has characteristics of both species.
John connected me with faculty in the Department of Bacteriology whom I could interact with and who understood some of the ideas behind the work. That’s how I did my Ph.D. in a different field. When a member of the faculty gives you freedom to do something, even if it is not their core area of a subject, and they respect a graduate student to do what they like to do although it is not a part of the program in the department, I think that’s very exciting and gives you freedom to think differently. And it also gives you the mindset to think differently in life. And then you know you can take a risk, you can do something different, whatever you like to. That helps in business also.
Where did this academic pivot take you next?
My experience at CALS led me to accept a National Institutes of Health fellowship at the Medical University of South Carolina in Charleston to work on signal transduction. There, I was asking questions related to the medical industry and using an indirect method of analysis, a genetics approach. If I take out a gene, is the cellular signal blocked? And if the signal is blocked, what happens to the cells? That’s what my publications were about.
How else did your time at CALS prepare you for your career?
I had one course, a scientific methods course, with [now professor emeritus] John Andrews. That course was hypothesis driven. How do you do science? You hypothesise, you test and experiment, and then you make a good sub-hypothesis, and again, you test. And what do you do in business? Same thing. You make one business plan; if it doesn’t work out, you make another one, and if it doesn’t work, you make another one. So it’s the same. A scientific methods course in a plant pathology department is very similar to business, to what you see in life. I realise this now; I was not realising it then.
How has Bharat Biotech developed low-cost vaccines?
We always look at it this way, what can be done for society and for people?
Our rotavirus vaccine, ROTAVAC, was part of the Indo-US Vaccine Action Program (VAP), a bilateral social innovation program between the two governments of India and the U.S. In 1998, I said I wanted to work with the rotavirus for two reasons. One, no vaccine innovation had ever been made in India. Number two, 300,000 children were dying per year in India because of diarrhoea caused by rotavirus.
And then, in 2001, we were the first company funded by the Bill and Melinda Gates Foundation for this project. This was the first efficacy trial in the developing world, so we were showing the country and the developing world that an efficacy trial can be done in India the way it is done in the U.S. and Europe.

In the vaccine field, the major cost is not the fundamental science, it’s the clinical research. Almost 80% of the cost of our project was for the clinical research program. We funded ours thanks to the Gates Foundation. And the Indo-US VAP program brought the best experts in the world, so we brought the same quality standards of the U.S. to India. Now we sell the vaccine at $1, and the same vaccine is sold in the U.S. at $68. We are now the largest rotavirus vaccine manufacturer in the world.
Our universal COVID-19 vaccine, COVAXIN, is also a fine example of success through public-private partnership.
What makes COVAXIN different from other COVID-19 vaccines?

For the COVID vaccine, I was always looking at one thing: safety, safety, safety. It’s the first criterion. Efficacy can come a little later. If safety is compromised and efficacy is good, it’s not good for the world. For people, safety is important. We chose an inactivated vaccine. So you just grow the live virus in the lab, and then you kill the RNA. The difference between a vaccine and a live virus is RNA. The live virus will have RNA; in the inactivated vaccine, the RNA is destroyed but all structurally safe, so it cannot multiply.
To do this, you need Biosafety Level 3 (BSL-3) containment because the live virus is so contagious. BSL-3 labs are all over the world, but not BSL-3 production facilities. We were the first company in the world to create a BSL-3 production facility for a polio vaccine project. So, when COVID came, we shut down the polio operation, and we switched over to a COVID vaccine. Scaling up capacities for inactivated vaccines is very limited, but the safety is the best. You give children three inactive injectable polio vaccines: three doses for lifetime immunity. You don’t give the vaccine again and again for a child, except the flu vaccine. That is exactly what we created with COVAXIN. It has a high T-cell response, so it has a long memory, lifetime protection.
Biosafety labs are specialised facilities where research is conducted on infectious agents. The labs are ranked from 1 to 4 based on the potential threat posed by the organisms they study, and safety measures are enhanced with each level.
This interview was first featured in Grow Magazine.


